How Hormonal Changes During Menopause Affect It
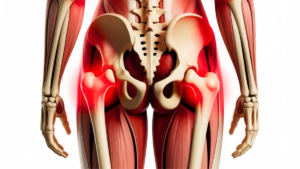
Back pain is one of the most common physical complaints among women over 40. Many notice that discomfort in the lower or upper back appears more frequently during midlife, sometimes becoming persistent and harder to ignore. While posture and daily habits play a role, hormonal changes during menopause are often an overlooked factor behind this type of pain.
As estrogen levels decline, the body undergoes muscular, skeletal, and metabolic changes that directly affect spinal health. Understanding this connection is essential for managing back pain more effectively during menopause. 👉Related article: https://mariahchic.com/menopause/sarcopenia-in-menopause
Why Back Pain Becomes More Common During Menopause?

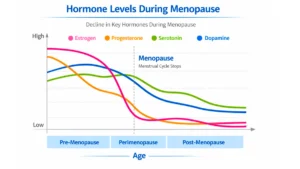
Menopause is marked by a gradual reduction in estrogen, a hormone that plays a protective role far beyond reproductive health.
Estrogen influences muscle tone, bone density, joint lubrication, and inflammation control.
As hormone levels fall, several changes may contribute to back pain, including:
-
reduced muscle strength
-
loss of bone density
-
increased systemic inflammation
-
decreased spinal stability
-
postural changes
Together, these factors increase stress on the spine and surrounding structures.
Our social network: https://www.youtube.com/watch?v=_B8oOIN1J2Q
Hormonal Decline and Muscle Loss
One of the key contributors to back pain during menopause is age-related muscle loss, known as sarcopenia. Muscles surrounding the spine are essential for posture, balance, and shock absorption. When muscle mass and strength decline, the spine becomes more vulnerable to overload and strain.
Weakened muscles also tend to become tense more easily, leading to stiffness and discomfort, particularly in the morning or after long periods of inactivity.
Bone Health, the Spine, and Menopause
Estrogen is crucial for maintaining bone density. During menopause, bone resorption accelerates, increasing the risk of osteopenia and osteoporosis. Even before a formal diagnosis, subtle bone loss can affect spinal integrity.
Reduced bone density in the vertebrae may lead to:
-
chronic lower back pain
-
spinal stiffness
-
postural changes
-
increased susceptibility to compression-related discomfort
Maintaining bone health becomes essential to preserving spinal stability and preventing long-term complications. Our social network: https://pt.pinterest.com/pin/1119426051144786943
Weight Gain and Its Impact on Back Pain

Weight gain is common during menopause due to hormonal shifts and metabolic changes. Excess body weight places additional mechanical stress on the spine, particularly the lumbar region.
Abdominal fat can alter posture and center of gravity, increasing pressure on the lower back. Over time, this added load may worsen existing pain or contribute to new discomfort. 👉 Related article: https://mariahchic.com/menopause/menopause-and-weight-gain
Lack of Physical Activity and Spinal Health
Decreased physical activity is another factor that may intensify back pain during menopause. Sedentary behavior leads to muscle weakening, reduced flexibility, and poorer joint mobility.
Our social network: https://www.youtube.com/watch?v=_B8oOIN1J2Q
Without regular movement, the muscles that support the spine lose strength and endurance, making everyday activities more physically demanding and increasing the risk of pain and stiffness.
The Role of a Balanced Diet in Managing Back Pain
A balanced diet supports both muscle and bone health, which are critical during menopause. Nutrient deficiencies can exacerbate fatigue, muscle weakness, and inflammation.
Dietary patterns that emphasize whole foods, adequate protein, calcium, vitamin D, and anti-inflammatory nutrients help maintain musculoskeletal health and support recovery. Limiting ultra-processed foods and excess sugar may also help reduce inflammation-related discomfort. 👉 Related article: https://mariahchic.com/menopause/bone-density-with-bone
Inflammation and Back Pain During Menopause

Estrogen helps regulate inflammatory responses in the body. As levels decline, low-grade chronic inflammation may increase, affecting muscles, joints, ligaments, and spinal discs.
This inflammatory state can manifest as diffuse back pain, muscle tension, and prolonged stiffness, especially when combined with poor sleep or high stress levels.
How to Manage Back Pain During Menopause
Back pain should not be dismissed as a normal consequence of aging. A comprehensive approach is essential, including:
-
medical evaluation and routine exams
-
muscle-strengthening and mobility exercises
-
weight management strategies
-
posture awareness
-
balanced nutrition
-
stress and sleep management
Individualized care allows women to address the underlying causes rather than only masking symptoms. 👉 Related article: https://mariahchic.com/menopause/menopause-body
Conclusion
Back pain in middle-aged women is often the result of interconnected hormonal, muscular, and skeletal changes that occur during menopause. Declining estrogen levels affect muscle strength, bone density, inflammation, and body composition, all of which influence spinal health.
Recognizing menopause as a contributing factor empowers women to seek appropriate care and adopt lifestyle strategies that promote comfort, mobility, and long-term wellbeing.
Scientific Studies
-
Low back pain and the menopausal transition
Published in 2015 – Menopause: The Journal of The North American Menopause Society -
Estrogen deficiency, bone loss, and musculoskeletal pain in midlife women
Published in 2018 – Journal of Women’s Health
Written and reviewed by: Dr. Vilma Mendonça
Image Bank: Pexels